MORPHINE
- CAS NO.:57-27-2
- Empirical Formula: C17H19NO3
- Molecular Weight: 285.34
- MDL number: MFCD00153032
- EINECS: 200-320-2
- SAFETY DATA SHEET (SDS)
- Update Date: 2025-01-27 09:38:02

What is MORPHINE?
Absorption
Morphine is absorbed in the alkaline environments of the upper intestine and rectal mucosa. The bioavailability of morphine is 80-100%. There is significant first-pass metabolism, therefore oral doses are 6 times larger than parenteral doses to achieve the same effect. Morphine reaches steady-state concentrations after 24-48 hours. Parenteral morphine has a Tmax of 15 minutes and oral morphine has a Tmax of 90 minutes, with a Cmax of 283nmol/L. The AUC of morphine is 225-290nmol*h/L.
Toxicity
The LD50 is 0.78μg/mL in males and 0.98μg/mL in females.
Patients experiencing an overdose present with respiratory depression, somnolence, skeletal muscle flaccidity, cold and clammy skin, miosis, and mydriasis. Symptoms of overdose can progress to pulmonary edema, bradycardia, hypotension, cardiac arrest, and death. Treat overdose with symptomatic and supportive treatment which may include the use of oxygen, vasopressors, and naloxone.
Description
Morphine is the principal alkaloid obtained from opium. Opium is the resinous latex that exudes from the seed pod of the opium poppy, Papver somneferum, when it is lacerated. Alkaloids account for approximately 25% of opium, and of this 25% about 60% is morphine.
Description
Morphine is the most important alkaloid in opium, an extract of the poppy?Papaver somniferum. A good grade of opium contains 9–14% of anhydrous morphine. It has been used as a potent painkiller for more than 150 years, especially after the development of the hypodermic needle. But it is extremely addictive and withdrawal is difficult.
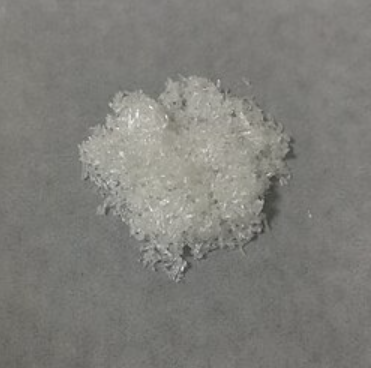
Chemical properties
White, crystalline alkaloid. Slightly soluble in water,alcohol, and ether.
Physical properties
Appearance: white or almost white crystalline powder or colorless, silky needles or cubical masses, efflorescent in a dry atmosphere. Solubility: soluble in water, slightly soluble in ethanol, practically insoluble in chloroform or ether. Specific optical rotation: ?110.0° to 115.0°
Originator
Avinza,Aetna Inc.
History
Morphine has a strong analgesic effect, especially for moderate and severe cancer pain. However, morphine has serious side effects, such as addiction, respiratory depression, acute poisoning, and death. Therefore, in regulating the clinical application of morphine at the same time, it is necessary to explore the alternative to morphine with strong analgesic role and minor side effects.
In the 1970s, tramadol was launched and marketed as “Tramal” by the German pharmaceutical company Grünenthal GmbH in West Germany , and 20 years later, it was launched in countries such as the United Kingdom, the United States, and Australia. It is marketed in many brand names worldwide. After R&D of more than 100 years, opioid drugs were increased and have been widely used in clinic as analgesic drugs.
The Uses of MORPHINE
A degradation product of Morphine. A dimolecular base formed by the gentle oxidation of Morphine in alkaline solution. Name Pseudomorphine is also used for the C17 alkaloid base
The Uses of MORPHINE
Morphine is the most important opium alkaloid,found in the poppy plant (Papaver somniferumL.). It is obtained by extracting thedried latex of poppy. It is also obtained fromopium, which is an air-dried milky exudate ofthe same plant produced by incising unripecapsules. Opium contains about 9–14% ofmorphine. It is used in medicine for its narcoticanalgesic, anesthetic, and pain-reliefactions.
The Uses of MORPHINE
Once morphine had been determined to be the principal pain-killing ingredient in opium, it was substituted for opium in many treatments. Morphine's analgesic ability is due to its ability to bind and activate opioid receptors in the central nervous system (brain and spinal cord).hen morphine or another opioid analgesic binds to the opioid receptors, it reduces the neurological transfer of pain signals to the brain. Morphine mimics natural pain relievers produced by the body called endorphins. When these natural pain-relieving compounds were discovered in the 1970s, the word endorphin was coined from the words endogenous and morphine.
Indications
Morphine is used for the management of chronic, moderate to severe pain.
Opiods, including morphine, are effective for the short term management of pain. Patients taking opioids long term may need to be monitored for the development of physical dependence, addiction disorder, and drug abuse.
Background
Morphine, the main alkaloid of opium, was first obtained from poppy seeds in 1805. It is a potent analgesic, though its use is limited due to tolerance, withdrawal, and the risk of abuse. Morphine is still routinely used today, though there are a number of semi-synthetic opioids of varying strength such as codeine, fentanyl, methadone, hydrocodone, hydromorphone, meperidine, and oxycodone.
Morphine was granted FDA approval in 1941.
Definition
ChEBI: A morphinane alkaloid that is a highly potent opiate analgesic psychoactive drug. Morphine acts directly on the central nervous system (CNS) to relieve pain but has a high potential for addiction, with tolerance and both physical and psychological dependen e developing rapidly. Morphine is the most abundant opiate found in Papaver somniferum (the opium poppy).
Definition
morphine: An opiate that is themain active constituent of opium. Itis used medically in the relief of severepain, and can be acetylated toproduce heroin. Morphine can be detected by the Marquis test.
Production Methods
Morphine is detoxified or biotransformed mainly in the liver by conjugation with glucuronic acid. Morphine is conjugated by a series of reactions involving the formation of uridine diphosphoglucose (UDP-glucose), the oxidation of carbon-6 of glucose to form uridine diphosphoglucuronic acid (UDP-glucuronic acid) and the transfer of glucuronic acid to morphine to form the morphine glucuronide. The following enzymes catalyze the sequential reactions; reaction(1), UDP-glucose pyrophosphorylase; reaction (2), UDP-glucose dehydrogenase; reaction (3), glucuronyl transferase; reaction (4) nucleoside diphosphokinase.
Indications
Morphine is mainly used to treat both acute and chronic severe pain. It is also used for pain caused by myocardial infarction and for labor pains. Morphine relieves pulmonary edema symptoms; anesthesia and preoperative administration can make the patient quiet and drowsy; compound formula of morphine was used for acute and chronic diarrhea.
Manufacturing Process
Morphin was extracted from the plant vegetable (the poppy) by the mixture of
water and methanol or the aqueous solution of potassium pyrosulfate. The
precipitation of the morphin was carried out by addition to the extract the
aqueous solution of sodium carbonate.
Morphin can be obtained from the extract by using the cation exchanger.
Free base of morphin was transformated to the sulfate salt.
brand name
Astramorph (AstraZeneca); Avinza (Ligand); Depodur (Skyepharma); Duramorph (Baxter Healthcare); Infumorph (Baxter Healthcare); Kadian (Alpharma); Ms Contin (Purdue Frederick); Oramorph (Xanodyne).
Therapeutic Function
Narcotic analgesic, Sedative
Acquired resistance
It is important to remember that a minor change in the structure of morphine (or any other opioid) will likely cause a different change in the affinity and intrinsic activity of the new compound at each of the opioid receptor types. Thus, the opioid receptor selectivity profile of the new compound may be different than the structure from which it was made or modeled (i.e., a selective μ agonist may shift to become a selective κ agonist, etc.). In addition, the new compound will have different physicochemical properties than its parent. The different physicochemical properties (e.g., solubility, partition coefficient, and pKa) will result in different pharmacokinetic characteristics for the new drug and can affect its in vivo activity profile. For example, a new drug (Drug A) that is more lipophilic than its parent may distribute better to the brain and appear to be more active, whereas in actuality, it may have lower affinity or intrinsic activity for the receptor. The greater concentration of Drug A reaching the brain is able to overcome its decreased agonist effect at the receptor.
Hazard
Narcotic, habit-forming drug, salerestricted by law in the U.S.
Health Hazard
Morphine is a habit-forming substance leadingto strong addiction. It exhibits acutetoxicity of several types and complexity.Morphine simultaneously produces depressingand stimulating actions on the centralnervous system. Depression of the centralnervous system results in drowsinessand sleep. Large doses may produce comaand lowering of heart rate and blood pressure.Initial doses of morphine may producestimulant action, inducing emesis, whichcan cause nausea and vomiting. Subsequentdoses may block emesis. The varietyof effects on the central nervous systemare manifested by behavioral changes rangingfrom euphoria and hallucinations tosedation. Repeated dosing enhances toleranceand dependence, with increasinglylarger doses needed to produce the effectof euphoria. Thus any abrupt terminationto morphine intake after chronic use maylead to physiological rebound (Hodgsonet al. 1988). Haffmans and associates (1987)reported the combating action of phelorphanagainst morphine addiction in chronicmorphine-dependent rats. Administration ofphelorphan (158 mmol/2 mL), an inhibitorof enzymes involved in the biodegradation ofenkephalins, affected the withdrawal symptomsin the addicted animals.
Severe morphine poisoning may result inrespiratory failure after fainting fits, accompaniedby coma and acute miosis. It exertseffects on the gastrointestinal tract, decreasingthe spasmotic reflexes in the intestinaltract, thus resulting in constipation.
LD50 value, oral (mice): 524 mg/kgLD50 value, subcutaneous (mice): 220 mg/kg
A fatal dose in humans may be about0.5–1 g.
Girardot and Holloway (1985) have investigatedthe effect of cold-water immersionon analgesic responsiveness to morphine inmature rats of different ages. This study indicatesthat chronic stress affects the reactivityto morphine in young mature rats but not inold rats.
Studies show that when coadministeredwith morphine, certain substances potentiatedmorphine’s toxicity or mortality in rats.These substances include gentamicin [1403-66-3] (Hurwitz et al. 1988), and doxorubicin(Adriamycin) (Innis et al.1987).
Stroescu and coworkers (1986) havereported the influence of the body’s electrolytecomposition on the toxic effect of morphine.In mice, depletion of body sodiumion increased the toxicity, which was foundto decrease by sodium loading. Glutathionedepletors such as cocaine, when coadministeredwith an opiate such as morphine orheroin, may enhance hepatotoxicity in humans(McCartney 1989). Such a potentiation effecthas been explained by the authors as being aresult of depletion of endogenous glutathione,which conjugates with morphine to preventtoxic interaction with hepatic cells.
Ascorbic acid and sodium ascorbate havebeen reported to prevent toxicity of morphinein mice (Dunlap and Leslie 1985). Sodiumascorbate (1 g/kg) injected intraperitoneally10 minutes before morphine (500 mg/kg)protected the animals against mortality dueto respiratory depression. These investigatorspostulated that ascorbate antagonized thetoxicity of morphine by selectively affectingthe neuronal activity.
Contact allergens
Morphine bitartrate caused contact dermatitis in a worker at a plant producing opium alkaloids. Morphine hydrochloride and morphine bitartrate showed patchtest- positive reactions in another patient with contact dermatitis working in the production of concentrated poppy straw. We observed a concomitant reaction between a morphine base and a codeine base in a patient with drug skin eruption due to codeine.
Pharmacokinetics
Morphine binding to opioid receptors blocks transmission of nociceptive signals, signals pain-modulating neurons in the spinal cord, and inhibits primary afferent nociceptors to the dorsal horn sensory projection cells.
Morphine has a time to onset of 6-30 minutes. Excess consumption of morphine and other opioids can lead to changes in synaptic neuroplasticity, including changes in neuron density, changes at postsynaptic sites, and changes at dendritic terminals.
Intravenous morphine's analgesic effect is sex dependent. The EC50 in men is 76ng/mL and in women is 22ng/mL.
Morphine-6-glucuronide is 22 times less potent than morphine in eliciting pupil constriction.
Pharmacokinetics
Morphine is the prototype opioid. It is selective for μ opioid receptors. The structure of morphine is composed of five fused rings, and the molecule has five chiral centers with absolute stereochemistry 5(R), 6(S), 9(R), 13(S) and 14(R). The naturally occurring isomer of morphine is levo-[(–)] rotatory. (+)-Morphine has been synthesized, and it is devoid of analgesic and other opioid activities.
Pharmacology
Morphine is subject to extensive first-pass metabolism; only 40–50% of the dose
reaches the central nervous system when taken orally. Morphine is metabolized primarily in the liver, and approximately 87% of a dose is excreted in the urine after 72?h
of administration. Morphine is metabolized primarily into morphine-3-glucuronide and morphine-6-glucuronide via glucuronidation by phase II metabolism enzyme
UDP-glucuronosyl transferase-2B7. The half-life is about 2.5–3.5?h .
Morphine, as an agonist of opioid receptor, has many pharmacological effects:
1. Analgesic: morphine can activate the opioid receptor and produce strong analgesic effect by simulating the role of endogenous enkephalin. It is better for persistent dull pain than intermittent sharp pain and visceral cramps.
2. Sedation: in the analgesic at the same time, there is a clear sedative effect, sometimes produce euphoria, which can improve the tension of the patient.
3. Respiratory depression: morphine can inhibit the respiratory center and reduce
the sensitivity of the respiratory center to carbon dioxide. The inhibition degree
of breathing is parallel to the dose of morphine, and excessive doses can cause
respiratory failure or death.
4. Antitussive: morphine can inhibit the cough center, resulting in antitussive effect.
5. Excited smooth muscle: morphine can excite the digestive tract smooth muscle,
leading to constipation, and increase tension of bile duct, ureter, and bronchial
smooth muscle.
6. The cardiovascular system: morphine can promote the release of endogenous
histamine and lead to peripheral vascular dilatation, blood pressure decrease,
cerebrovascular expansion, and intracranial pressure increase.
7. Antiemetic and miotic effect: morphine can play antiemetic effect through the
central nervous system, and the most important feature with morphine application is the pinhole-like pupil.
Pharmacology
Morphine is a relatively hydrophilic phenanthrene derivative. It may be given orally (immediate or modified release), rectally, topically, parenterally and via the neuraxial route. The standard parenteral dose for adults is 10mg, although many factors affect this and the dose should be titrated to effect. I ts oral bioavailability is dependent on first-pass hepatic metabolism and may be unpredictable (35%–75%). S ingle-dose studies of morphine bioavailability indicate that the relative potency of oral to intramuscular morphine is 1:6, although with repeated regular administration, this ratio becomes approximately 1:3. The dose of short-acting morphine for breakthrough pain should be approximately one-sixth of the total daily dose. Morphine has a plasma half-life of approximately 3 h and duration of analgesia of 4–6 h. Morphine is metabolised, at least in part, by microsomal UDP glucuronyl transferases (UDPGT) in the liver, kidney and intestines. Several of these metabolites may have clinically significant effects. Although morphine conjugation occurs in the liver, extrahepatic sites may also be important, such as the kidney and GI tract. The site of conjugation on the molecule also varies, leading to a variety of metabolites. After glucuronidation, metabolites are excreted in urine or bile, dependent on molecular weight and polarity; more than 90% of morphine metabolites are excreted in the urine. The main metabolite in humans is morphine-3- glucuronide (60%–80%), and this may have an excitatory effect via CNS actions not related to opioid receptor activation. Morphine-6-glucuronide (M- 6-G) is active at the MOP receptor, producing analgesia and other MOP related effects. I t is significantly more potent than morphine. Therefore M-6- G produces significant clinical effects despite only 10% of morphine being metabolised in this way. A s it is excreted via the kidneys, it may accumulate in patients with impaired renal function, causing respiratory depression. A ccumulation of morphine metabolites, especially M-6-G, may become significant when creatinine clearance declines to 50 ml min–1 or less.
Clinical Use
Morphine remains the standard by which other analgesic
drugs are compared. The predominant effects of
morphine are at the μ-opioid receptor, although it interacts
with other opioid receptors as well. Morphine is
indicated for the treatment of moderate to severe and
chronic pain. It is useful preoperatively for sedation,anxiolytic effects, and to reduce the dose of anesthetics.
Morphine is the drug of choice for the treatment of
myocardial infarction because of its bradycardiac and
vasodilatory effects. In addition, morphine is the most
commonly used drug for the treatment of dyspneaassociated
pulmonary edema. It is thought that morphine
reduces the anxiety associated with shortness of
breath in these patients along with the cardiac preload
and afterload.
The use of morphine via the oral route has drawbacks
because of its first-pass effect; however, oral morphine
has been recommended for use in cancer patients
for its ease of administration. In particular, the longacting
preparations of morphine, such as MS-Contin
and Ora-Morph, are described as the cornerstone of
pain treatment in cancer patients, either alone or in
combination with nonopioids.
Morphine is the most commonly used analgesic drug
administered via the epidural route because it is potent,
efficacious, and hydrophilic. The more hydrophilic the
drug, the slower the onset and the longer the duration
of action following epidural administration. Single-dose
or continuous infusion of morphine is used to provide
pain relief in thoracic and abdominal surgical patients
and in cancer patients at high risk for developing side
effects associated with systemic opioids. Since morphine
does not produce anesthesia via the epidural route, the
patient is able to move about normally; motor function
is preserved.The drawback to epidural use of morphine
is that certain types of pain are relatively unresponsive,
such as that associated with visceral stimuli, as in pancreatitis,
and neuropathic pain from nerve deafferentation.
In addition, patients can develop respiratory depression
and nausea from the rostral flow of the drug to
medullary centers, although the effects are much less severe
than those observed following the systemic administration
of the drug, and can be alleviated by elevation
of the head of the patient at a 30-degree angle. Patients
may also itch because of histamine release.
Patient-controlled analgesia (PCA) is an alternative
method of administration of morphine.The use of an indwelling
catheter allows the patient to administer the
drug at frequent intervals for pain relief. PCA systems
allow patients the freedom to assess the need for their
own analgesia and to titrate a dose tailored to their
needs. Dependence is rarely observed in patients using
PCA for acute pain management.
Side Effects
The opioids generally have a high level of safety when
used in therapeutic dosages. However, there are several
notable exceptions. Morphine and other opioids are
contraindicated in patients with hypersensitivity reactions
to the opioids. In addition, morphine should not be
used in patients with acute bronchial asthma and should not be given as the drug of first choice in patients with
pulmonary disease, because it has antitussive effects
that prevent the patient from clearing any buildup of
mucus in the lungs. Opioids with less antitussive effects,
such as meperidine, are better for such situations.
When used via the epidural route, the site for injection
must be free of infection. In addition, the use of
corticosteroids by the patient should be halted for at
least 2 weeks prior to the insertion of the catheter to
prevent infection, since morphine increases the immunosuppressive
effects of the steroids.
Opioids are contraindicated in head trauma because
of the risk of a rise in intracranial pressure from vasodilation
and increased cerebrospinal fluid volume. In addition,
in such patients the onset of miosis following opioid
administration can mask the pupillary responses
used diagnostically for determination of concussion.
The clearance of morphine and its active metabolite,
morphine-6-glucuronide depends on adequate renal
function. The elderly are particularly susceptible to accumulation
of the drugs, hence respiratory depression
and sedation. Morphine, like all opioids, passes through
the placenta rapidly and has been associated with prolongation
of labor in pregnant women and respiratory
depression in the newborn.
Morphine and other opioids exhibit intense sedative
effects and increased respiratory depression when combined
with other sedatives, such as alcohol or barbiturates.
Increased sedation and toxicity are observed
when morphine is administered in combination with
the psychotropic drugs, such as chlorpromazine and
monoamine oxidase inhibitors, or the anxiolytics, such
as diazepam.
Respiratory depression, miosis, hypotension, and
coma are signs of morphine overdose.While the IV administration
of naloxone reverses the toxic effects of
morphine, naloxone has a short duration of action and
must be administered repeatedly at 30- to 45minute intervals
until morphine is cleared from the body.
Safety Profile
Poison experimentally
by ingestion, intracerebral, intraperitoneal,
subcutaneous, and intravenous routes.
Human reproductive effects by an
unspecified route: effects on newborn,
including drug dependence. Experimental
reproductive effects. Mutation data
reported.
Morphine is the constituent of opium most responsible for its toxic effects. When
taken orally, the effects of morphine
poisoning begin to appear in 20-40 minutes;
if taken hypodermically, the symptoms
appear much earlier and narcotism is more
likely to follow the early symptoms. Abuse
leads to habituation or adlction. Inlvidual
susceptibility varies greatly and children are
more susceptible than adults. When heated
to decomposition it emits toxic fumes of
NOx.
Drug interactions
Potentially hazardous interactions with other drugs
Analgesics: possible opioid withdrawal with
buprenorphine and pentazocine.
Antibacterials: metabolism increased by rifampicin.
Antidepressants: possible CNS excitation or
depression with MAOIs - avoid concomitant use,
and for 2 weeks after stopping MAOI; possible
CNS excitation or depression with moclobemide;
increased sedative effects with tricyclics.
Antiepileptics: increases bioavailability of
gabapentin.
Antihistamines: increased sedative effects with
sedating antihistamines.
Antipsychotics: enhanced hypotensive and sedative
effects.
Antivirals: concentration possibly reduced by
ritonavir.
Dopaminergics: avoid with selegiline.
Nalmefene: avoid concomitant use.
Sodium oxybate: enhanced effect of sodium oxybate
- avoid.
Metabolism
Morphine is 90% metabolized by glucuronidation by UGT2B7 and sulfation at positions 3 and 6. Morphine can also be metabolized to codeine, normorphine, and morphine ethereal sulfate.
Metabolism
Extensive first-pass metabolism in the liver and gut. The majority of a dose of morphine is conjugated with glucuronic acid in the liver and gut to produce morphine 3-glucuronide and morphine-6-glucuronide (active). Other active metabolites include normorphine, codeine, and morphine ethereal sulphate. After an oral dose, about 60% is excreted in the urine in 24 hours, with about 3% excreted as free morphine in 48 hours. After a parental dose, about 90% is excreted in 24 hours, with about 10% as free morphine, 65-70% as conjugated morphine, 1% as normorphine and 3% as normorphine glucuronide. Up to 10% of a dose may be excreted in the bile.
Purification Methods
Crystallise the narcotic from MeOH or anisole. It dehydrates at 130o. Its solubility in H2O is 0.2g/L at 20o and 0.9g/L at 100o, and in EtOH it is 5g/L at 20o and 10g/L on boiling. The styphnate has m 189o (from aqueous EtOH). [Beilstein 27 II 118, 27 III/IV 2223.]
References
Derosne., Ann. Chirn., 45, 257 (1803)
Laurent., Ann. Chirn. Phys., 19, iii, 359 (1847)
Muller., Apoth. Zeit., 18, 257 (1903)
Mannich., Chern. Zentr., II, 820 (1916)
Emde., Helv. Chirn. Acta, 13, 1035 (1930)
Gates, Tschudi., 1. Arner. Chern. Soc., 78, 1380 (1956)
Crystal structure:
MacKay, Hodgkin., 1. Chern. Soc., 3261 (1955)
Synthesis:
Gates, TschudL,J. Arner. Chern. Soc., 74, 1109 (1952)
Elad, Ginsburg., ibid, 76,312 (1954)
Elad, Ginsburg., J. Chern. Soc., 3052 (1954)
Morrison, Waite, Shavel., Tetrahedron Lett., 4055 (1967)
NMR and mass spectra:
Rull., Bull. Soc. Chim. Fr., 586 (1963)
Okuda et al., Chern. Pharrn. Bull. (Tokyo), 11, 1465 (1963)
Wheeler, Kinstle, Rinehart., J. Arner. Chern. Soc., 89,4494 (1967)
Biosynthesis:
Barton et aI., J. Chern. Soc., 2423 (1965)
Pharmacology:
Vahlen., Arch. expo Path. Pharrn., 47, 368 (1902)
Small et al., Public Health Reports, Suppl. 138, Washington (1938)
Krueger, Eddy, Sumwalt., ibid, No. 165, Washington (1943)
Properties of MORPHINE
| Melting point: | 255°C |
| Boiling point: | 427.77°C (rough estimate) |
| Density | 1.0864 (rough estimate) |
| refractive index | 1.5400 (estimate) |
| Flash point: | 11 °C |
| storage temp. | −20°C |
| solubility | Ethanol (Slightly), Methanol (Slightly) |
| pka | 8.21(at 25℃) |
| form | Solid |
| color | White to Pale Yellow |
| Water Solubility | 0.4mg/L(25 ºC) |
| CAS DataBase Reference | 57-27-2 |
| EPA Substance Registry System | Morphinan-3,6-diol, 7,8-didehydro-4,5-epoxy-17-methyl- (5.alpha.,6.alpha.)- (57-27-2) |
Safety information for MORPHINE
| Signal word | Danger |
| Pictogram(s) |
 Flame Flammables GHS02  Skull and Crossbones Acute Toxicity GHS06  Health Hazard GHS08 |
| GHS Hazard Statements |
H225:Flammable liquids H370:Specific target organ toxicity, single exposure |
| Precautionary Statement Codes |
P210:Keep away from heat/sparks/open flames/hot surfaces. — No smoking. P280:Wear protective gloves/protective clothing/eye protection/face protection. P370+P378:In case of fire: Use … for extinction. P403+P235:Store in a well-ventilated place. Keep cool. |
Computed Descriptors for MORPHINE
New Products
Indole Methyl Resin tert-butyl 9-methoxy-3-azaspiro[5.5]undecane-3-carboxylate Boc-His(Boc)-OH 2-CTC Resin 4-Chloro-7-tosy1-7Hpyrrolo[2,3-d]pyrimidine 5,7-Dibromo-1H-indole 2,5-dichloro-N-hydroxy-4,6-dimethylpyridine-3-carboximidamide 2,2-Dimethoxy-7-azaspiro[3.5]nonane hydrochloride 4-chloromethyl-5-methyl-1,3-dioxol-2-one (DMDO-Cl) R-2-BENZYLOXY PROPIONIC ACID 1,1’-CARBONYLDIIMIDAZOLE 1,1’-CARBONYLDI (1,2-4 TRIAZOLE) N-METHYL INDAZOLE-3-CARBOXYLIC ACID 4-((2-hydroxyethyl)thio)benzoic acid 1-(TERT-BUTOXYCARBONYL)-2-PYRROLIDINONE Methyl 6-methylnicotinate 3-Pyridineacrylic acid tert-Butyl carbazate TETRAHYDRO-2H-PYRAN-3-OL 2-((4-morpholinophenylamino) (methylthio) methylene) malononitrile 3-(4-morpholinophenylamino)-5-amino-1H-pyrazole-4-carbonitrile 2,4-dihydroxybenzaldehyde 1,3-Diethyl-1,3-Diphenylurea Methyl 2-methylquinoline-6-carboxylateRelated products of tetrahydrofuran

You may like
-
 Pyridine 99.5% HPLC /UV SpectroscopyView Details
Pyridine 99.5% HPLC /UV SpectroscopyView Details
110-86-1 -
 Guanine , 99%View Details
Guanine , 99%View Details
73-40-5 -
 Piperazine Spot supply, best priceView Details
Piperazine Spot supply, best priceView Details
110-85-0 -
 Potassium Hydroxide 90%View Details
Potassium Hydroxide 90%View Details
1310-58-3 -
 Dibutyl PhthalateView Details
Dibutyl PhthalateView Details
84-74-2 -
 Imidazole Spot supply, competitive priceView Details
Imidazole Spot supply, competitive priceView Details
288-32-4 -
 Octadecyl 3-(3,5-di-tert-butyl-4-hydroxyphenyl)propionate 98% (GC)View Details
Octadecyl 3-(3,5-di-tert-butyl-4-hydroxyphenyl)propionate 98% (GC)View Details
2082-79-3 -
 Thiourea 99% ARView Details
Thiourea 99% ARView Details
62-56-6
