Metronidazole
Synonym(s):2-Methyl-5-nitroimidazole-1-ethanol;MTZ
- CAS NO.:443-48-1
- Empirical Formula: C6H9N3O3
- Molecular Weight: 171.15
- MDL number: MFCD00009750
- EINECS: 207-136-1
- SAFETY DATA SHEET (SDS)
- Update Date: 2025-12-23 21:30:31
What is Metronidazole?
Absorption
After the intravenous infusion of a 1.5g dose, peak concentration was reached within 1 hour and was peak level of 30-40 mg/L. When a multiple-dose regimen of 500mg three times a day administered intravenously, steady-state concentrations were achieved within about 3 days and peak concentration was measured at 26 mg/L.
When administered orally in the tablet form, metronidazole is absorbed entirely absorbed, showing a bioavailability of greater than 90%. One resource indicates that Cmax after a single oral dose of 500mg metronidazole ranges from 8 to 13 mg/L, with a Tmax of 25 minutes to 4 hours. The AUC following a single 500mg oral dose of metronidazole was 122 ± 10.3 mg/L ? h.
A note on the absorption of topical preparations
Insignificant percutaneous absorption of metronidazole occurs after the application of 1% metronidazole cream topically. Healthy volunteers applied one 100 mg dose of 14C-labelled metronidazole 2% cream to unbroken skin. After 12 hours, metronidazole was not detected in the plasma. Approximately 0.1% to 1% of the administered metronidazole was measured in the urine and feces.
Toxicity
LD50 information
The oral LD50 of metronidazole in rats is 5000 mg/kg
Overdose information
Adverse effects that may be exaggerated with an overdose include peripheral neuropathy, central nervous system toxicity, seizures, disulfiram-like effect (if combined with alcohol) dark urine, a metallic taste in the mouth, nausea, epigastric discomfort, and vertigo, in addition to neutropenia. There is no specific antidote for metronidazole overdose. Symptomatic and supportive treatment should be employed in addition to the administration of activated charcoal to remove the unabsorbed drug from the gastrointestinal tract. In addition to the above measures, contact the local poison control center for updated information on the management of a metronidazole overdose.
Description
Metronidazole is a nitroimidazole antibiotic first isolated in the 1950s. Many nitroimidazoles were being studied at the time, as the class was found to have trichomonacidal properties. Metronidazole was of particular interest due to its high activity against Trichomonas vaginalis and Entamoeba histolytica both in vitro and in vivo as well as clinical activity against many anaerobic pathogens including Gram-positive and Gramnegative bacteria and Giardia lamblia. Metronidazole is often used clinically for intra-abdominal infections and is the firstline treatment for Clostridium difficile–associated diarrhea.
Description
Metronidazole is a nitroimidazole anti-infective medication used mainly in the treatment of infections caused by susceptible organisms, particularly anaerobic bacteria and protozoa.
Chemical properties
Metronidazole is an odorless, white, yellow, or cream-colored crystalline solid. Darkens on exposure to light. Bitter, salty taste (do not test). Soluble in hot water, slightly soluble in ethanol, slightly soluble in water or chloroform, very slightly soluble in ether.
Originator
Flagyl,Specia,France,1960
The Uses of Metronidazole
Metronidazole is the drug of choice for amebiases, vaginal trichomonasis and trichlomonadic urethritis in men, lambliosis, amebic dysentery, and anaerobic infections caused by microorganisms that are sensitive to the drug. Synonyms of this drug are flagyl, protostat, trichopol, and vagimid.
The Uses of Metronidazole
Used as an antibacterial in the treatment of rosacea. Antiprotozoal (trichomonas). A potential human carcinogen.
The Uses of Metronidazole
Metronidazole is available as oral, intravaginal, topical, and parenteral preparations. It is manufactured by several companies, but is only available by prescription. Unintentional environmental exposure is unlikely, and if it occurs, it is very unlikely to cause toxicity.
The Uses of Metronidazole
Metronidazole, is an antibiotic and antiprotozoal agent. It is mainly used to treat or prevent systemic or local infections caused by anaerobic bacteria, such as anaerobic bacterial infections in the abdominal cavity, digestive tract, female reproductive system, lower respiratory tract, skin and soft tissues, bones and joints, etc. Inflammation, meningeal infections, and colitis caused by antibiotic use are also effective. Tetanus is often treated with tetanus antitoxin (TAT). It can also be used for oral anaerobic infection. On October 27, 2017, the list of carcinogens published by the World Health Organization's International Agency for Research on Cancer was preliminarily sorted for reference, and metronidazole was included in the list of class 2B carcinogens. In January 2020, metronidazole was selected into the second batch of national centralized drug procurement list.
Indications
Metronidazole is indicated for the treatment of confirmed trichomoniasis caused by Trichomonas vaginalis (except for in the first trimester of pregnancy) and the patient's sexual partners, bacterial vaginosis, certain types of amebiasis, and various anaerobic infections. The above anaerobic infections may occur on the skin and skin structures, the abdomen, the heart, reproductive organs, central nervous system, and the respiratory system. Some may also be present in the bloodstream in cases of septicemia. Common infections treated by metronidazole are Bacteroides species infections, Clostridium infections, and Fusobacterium infections, as well as Peptococcus and Peptostreptococcus infections. Topical formulations of metronidazole are indicated for the treatment of inflammatory lesions of rosacea.
It is also used off-label in the treatment of Crohn's disease, as a prophylactic agent after surgery, and in the treatment of Helicobacter pylori infection. It has also been studied in the prevention of preterm births and to treat periodontal disease.
Background
Metronidazole is a commonly used antibiotic, belonging to the nitroimidazole class of antibiotics. It is frequently used to treat gastrointestinal infections as well as trichomoniasis and giardiasis, and amebiasis which are parasitic infections. Metronidazole has been used as an antibiotic for several decades, with added antiparasitic properties that set it apart from many other antibacterial drugs, allowing it to treat a wide variety of infections. It is available in capsule form, tablet form, and topical form, and suppository preparations for the treatment of various infections.
What are the applications of Application
Metronidazole is an antibiotic affective against protozoa and anaerobic gram-positive and gram-negative bacteria.
Definition
ChEBI: Metronidazole is a member of the class of imidazoles substituted at C-1, -2 and -5 with 2-hydroxyethyl, nitro and methyl groups respectively. It has activity against anaerobic bacteria and protozoa, and has a radiosensitising effect on hypoxic tumour cells. It may be given by mouth in tablets, or as the benzoate in an oral suspension. The hydrochloride salt can be used in intravenous infusions. Metronidazole is a prodrug and is selective for anaerobic bacteria due to their ability to intracellularly reduce the nitro group of metronidazole to give nitroso-containing intermediates. These can covalently bind to DNA, disrupting its helical structure, inducing DNA strand breaks and inhibiting bacterial nucleic acid synthesis, ultimately resulting in bacterial cell death. It has a role as an antitrichomonal drug, a prodrug, an antibacterial drug, an antimicrobial agent, an antiparasitic agent, a xenobiotic, an environmental contaminant, a radiosensitizing agent and an antiamoebic agent. It is a member of imidazoles, a C-nitro compound and a primary alcohol. It is a conjugate base of a metronidazole(1+).
Indications
Metronidazole (Flagyl, Metrogel) exerts activity against most anaerobic bacteria and several protozoa.The drug freely penetrates protozoal and bacterial cells but not mammalian cells. Metronidazole can function as an electron sink, and because it does so, its 5-nitro group is reduced. The enzyme, pyruvate-ferredoxin oxidoreductase, found only in anaerobic organisms, reduces metronidazole and thereby activates the drug. Reduced metronidazole disrupts replication and transcription and inhibits DNA repair.
Manufacturing Process
2-Methyl-4(or 5)-nitroimidazole (127 g) is heated with ethylene chlorohydrin (795 g) for 18 hours at 128° to 130°C and the chlorohydrin (660 g) is then distilled under reduced pressure (30mm Hg). The residue is treated with water (300 cc) and filtered, and the filtrate is made alkaline by the addition of sodium hydroxide solution (d = 1.33, 100 cc). It is then extracted with chloroform (1,000 cc) and, after evaporation of the chloroform in vacuo, there is obtained a pasty mass (77 g) which is recrystallized from ethyl acetate (450 cc) in the presence of animal charcoal. There is thus obtained 1-(2- hydroxyethyl)-2-methyl-5-nitroimidazole (24 g) as a creamy white crystalline powder melting at 158° to 160°C.
brand name
Flagyl (Searle); Metrogel (Galderma); Metrogel (3M Pharmaceuticals); Noritate(Sanofi Aventis); Vandazole (Teva).
Therapeutic Function
Antiprotozoal
Antimicrobial activity
Metronidazole inhibits E. histolytica, G. lamblia, T. vaginalis, Blastocystis hominis, B. coli, and the helminth Dracunculus medinensis. It is also bactericidal for obligate anaerobic gram-positive and gram-negative bacteria except Actinomyces spp. It is not active against aerobes or facultative anaerobes. Drug resistance is infrequent; the mechanism of resistance is not understood. Tinidazole, a 5-nitroimidazole closely related to metronidazole, is effective against vaginal trichomoniasis resistant to metronidazole.
Acquired resistance
Although resistance in Bacteroides spp. and T. vaginalis is well documented, it is uncommon. Resistance occurs more frequently in H. pylori and failure of treatment with triple drug regimens may be associated with resistance to the metronidazole component.
General Description
White to pale-yellow crystalline powder with a slight odor. Bitter and saline taste. pH (saturated aqueous solution) about 6.5.
Air & Water Reactions
Insoluble in water.
Reactivity Profile
Metronidazole darkens on exposure to light. Metronidazole is incompatible with strong oxidizing agents. .
Fire Hazard
Flash point data for Metronidazole are not available; however, Metronidazole is probably combustible.
Pharmaceutical Applications
A 5-nitroimidazole available for oral administration or as a suppository; also formulated as the hydrochloride for intravenous use, and as the benzoate in an oral suspension and a dental gel. Aqueous solubility: 10 g/L at 20°C. Soluble in dilute acids. It is photolabile and preparations should be protected from light. Metronidazole hydrochloride has a low pH (0.5–2.0) when reconstituted, and reacts with aluminum in equipment, including needles, to produce a reddish-brown discoloration. It is incompatible with several agents and other drugs should not be added to intravenous solutions.
Contact allergens
Metronidazole is a nitro-6-imidazole compound with antiprotozoal and antibacterial properties. Topical exposure may induce allergic contact dermatitis. Sensitization is mainly observed with the treatment of rosacea and rarely occurs from handling of table.
Biochem/physiol Actions
Metronidazole is a prodrug and is selective for anaerobic bacteria due to their ability to intracellularly reduce metronidazole to its active form. Reduced metronidazole covalently binds to DNA which disrupts its helical structure, induces DNA strand breaks and inhibits bacterial nucleic acid synthesis. Bacterial cell death results.
Mechanism of action
Despite the availability of metronidazole since the late 1950s, the mechanism of action of the drug is still unknown. It generally is agreed that metronidazole is a pro-drug and that anaerobic organisms reduce the nitro group in metronidazole to a hydroxylamine, as shown in Figure 39.2, during which a reactive derivative or reactive species are produced that cause destructive effects on cell components (i.e., DNA, proteins, and membranes). Specifically, DoCampo has reported that nitroaryl compounds (nitroimidazoles, metronidazole; nitrofurans, nifurtomox) are reduced to nitro radical anions, which in turn react with oxygen to regenerate the nitroaryl and the superoxide radical anion. Further reduction of superoxide radical anion leads to hydrogen peroxide and homolytic cleavage of the latter leads to hydroxyl radical formation. Superoxide radical anion, hydrogen peroxide, and hydroxyl radicals are referred to as reactive oxygen species (ROS) and are the reactive substances that are implicated in damage to critical cellular components of the parasite.
Pharmacokinetics
Metronidazole treats amebiasis, trichomoniasis, and giardiasis, exerting both antibacterial and antiprotozoal activities. Metronidazole is an effective treatment for some anaerobic bacterial infections. Metronidazole has shown antibacterial activity against the majority of obligate anaerobes, however, during in vitro studies, it does not demonstrate significant action against facultative anaerobes or obligate aerobes. The nitro group reduction of metronidazole by anaerobic organisms is likely responsible for the drug's antimicrobial cytotoxic effects, causing DNA strand damage to microbes.
A note on convulsions and neuropathy and carcinogenesis
It is important to be aware of the risk of peripheral neuropathy and convulsions associated with metronidazole, especially at higher doses. If convulsions or numbness of an extremity occur, discontinue the drug immediately. Metronidazole has been found to be carcinogenic in mice and rats. The relevance to this effect in humans is unknown. It is advisable to only administer metronidazole when clinically necessary and only for its approved indications.
Pharmacokinetics
Oral absorption :>90%
Cmax 400 mg oral :c. 10 mg/L after 3–5 h
Plasma half-life: 6–11 h
Volume of distribution:0.6–1.1 L/kg
Plasma protein binding:<20%
absorption
Peak plasma concentrations after oral administration are proportional to the dose. Plasma levels are usually lower in men because of weight differences. In patients treated intravenously with a loading dose of 15 mg/kg followed by 7.5 mg/kg every
6 h, peak steady state plasma concentrations averaged 25 mg/L with minimum trough concentrations averaging 18 mg/L.
The bioavailability of metronidazole in rectal suppositories is around 60%. Effective blood concentrations occur 5–12 h after the first suppository and are maintained by an 8 h regimen.
There are conflicting data on the effects of age on absorption. One study, which did not distinguish between metronidazole and its metabolites, indicated that the area under the curve (AUC) for plasma was almost doubled in the elderly. However, the general consensus is that there is no requirement for a decreased dosage for the elderly, unless there is significant renal impairment.
Distribution
It is widely distributed in body tissues after oral or intravenous administration.It appears about 90 min after an oral dose in brain tissue, cerebrospinal fluid (CSF), saliva and breast milk in concentrations similar to those found in plasma: and in :vaginal secretions, pleural and prostatic fluid at levels about 40% of those of the plasma. In patients receiving 500 mg every 12 h or 1 g every 6 h, CSF levels of up to 2 and 8 mg/L, respectively, have been found. Bactericidal concentrations of metronidazole are achieved in pus from hepatic abscesses. Concentrations in placenta and fetal tissue are related to the corresponding maternal plasma levels: concentrations of 3.5 mg/kg (placenta) and 9 mg/kg (fetus) when the plasma concentration was 13.5 mg/L.
Metabolism
It is metabolized in the liver to a glucuronide conjugate and to acid and hydroxy derivatives. The acid metabolite, produced by oxidation of the N-1 ethanol side-chain, is microbiologically inactive and appears in the urine because of its high water solubility. The hydroxy derivative, which is as active as the parent drug against G. vaginalis, is formed by oxidation of the methyl group on C-2 of the imidazole ring, first to the hydroxymethyl derivative and subsequently to the carboxylic acid. Hydroxymetronidazole has a half-life of 10–13 h. Both metronidazole itself and the hydroxymethyl metabolite can form sulfate or glucuronide conjugates: the acid metabolite may be excreted as the glycine conjugate. Traces of metabolites derived from reduction of the nitro group are found in urine and are assumed to be formed by the intestinal flora.
excretion
About 60–80% of the dose appears in the urine and 6–15% in the feces. The hydroxy and acid metabolites are also excreted in the urine. Glucuronide conjugates account for approximately 20% of the total. Renal clearance is approximately 10 mL/min per 1.73 m2. Decreased renal function does not alter the single-dose kinetics and dose adjustment is not normally required in patients with renal impairment. However, the hydroxy metabolite may accumulate in patients with end-stage disease and dose reduction may be necessary. Elimination is prolonged in patients with impaired liver function necessitating dose reduction. Hemodialysis increases the clearance of metronidazole, shortening the half-life to 2–3 h.
Newborn infants possess a decreased capacity to eliminate metronidazole. In one study, the elimination half-life measured during the first 3 days of life was inversely related to gestational age. In premature newborns and infants whose gestational ages were between 28 and 40 weeks, the corresponding half-life elimination rates ranged from 10.9 to 22.5 h.
Pharmacology
Absorption from the intestinal tract is usually good. Food delays but does not reduce absorption.The drug is distributed in body fluids and has a half-life of about 8 hours. High levels are found in plasma and cerebrospinal fluid (CSF). Less than 20% binds to plasma proteins. Metronidazole is metabolized by oxidation and glucuronide formation in the liver and is primarily excreted by the kidneys, although small amounts can be found in saliva and breast milk. Dose reduction is generally unnecessary in renal failure.
Clinical Use
Metronidazole is the most effective agent available for
the treatment of individuals with all forms of amebiasis,
with perhaps the exception of the person who is asymptomatic
but continues to excrete cysts. That situation
calls for an effective intraluminal amebicide, such as
diloxanide furoate, paromomycin sulfate, or diiodohydroxyquin.
Metronidazole is active against intestinal
and extraintestinal cysts and trophozoites.
Although quinacrine hydrochloride has been used
for the treatment of giardiasis, many physicians prefer
metronidazole. Furazolidone is an alternate choice.
Metronidazole is the drug of choice in Europe for
anaerobic bacterial infections; concern about possible
carcinogenicity has led to some caution in its use in the
United States.Recently it has been found to be effective
in treating D. medinensis (Guinea worm) infections and
Helicobacter pylori.
Side Effects
precautions
Alcohol should not be taken during and for 48 h after therapy because of a possible disulfiram-like reaction, nor should it be combined with formulations containing alcohol. It should not be given in cases of known hypersensitivity to nitroimidazoles.
It enhances the anticoagulant effect of warfarin and may impair the clearance of phenytoin and lithium. Phenytoin may increase the metabolism of metronidazole. Plasma concentrations are decreased by the concomitant administration of phenobarbital (phenobarbitone). The drug may also mask the immunological response of untreated early syphilis cases because of its antitreponemal activity.
It should be used with care in patients with blood dyscrasias or with any central nervous system (CNS) disease.
The drug should be avoided in pregnancy, especially during the first trimester and particularly if high doses are being administered. Use during the second and third trimesters may be acceptable if alternative therapies for trichomoniasis have failed, but single-dose (2 g oral) therapy should be avoided. The drug may cause the breast milk to taste bitter. Breast feeding should be discontinued until 24 h after the last dose to allow excretion of the drug. It appears safe when given to nursing mothers at doses of up to 400 mg every 8 h.
adverse effects
An unpleasant sharp, metallic taste is not unusual. Furry tongue, glossitis and stomatitis have occurred; stomatitis may be associated with overgrowth of Candida spp. during treatment. Gastrointestinal disturbances include nausea, vomiting, abdominal discomfort and diarrhea, and occur with intravenous and oral preparations. Pseudomembranous colitis has also been reported.
Nervous system effects associated with intravenous and oral preparations include convulsive seizures, peripheral neuropathy, dizziness, vertigo, incoordination, ataxia, confusion, irritability, depression, weakness and insomnia. Peripheral neuropathy was found in 11 of 13 patients aged 12–22 years treated for Crohn’s disease. The symptoms disappeared when the dose was discontinued or markedly reduced. Peripheral neuropathy or CNS toxicity is more likely in patients treated for 10 days or more and treatment should be discontinued. The co-administration of cimetidine increases plasma levels of metronidazole and may increase the risk of neurological side effects.
Reversible neutropenia has been reported after administration of both intravenous and oral preparations. Bone marrow aplasia and thrombocytopenia are rare. Hemolytic uremic syndrome was reported in six children who had been given metronidazole for non-specific diarrhea or for prophylaxis after bowel surgery.
Erythematous rash and pruritus have been reported after use of the intravenous preparation. The risk of thrombophlebitis can be minimized by avoiding prolonged indwelling catheters for intravenous infusion.
Rarely, flattening of the T wave may be seen in electrocardiographic tracings. A number of cases of deafness have been reported. Myopia related to 11 days’ oral treatment for trichomoniasis disappeared 4 days after treatment was stopped, but returned when treatment was resumed. There have been isolated reports of pancreatitis and gynecomastia.
Side Effects
The most frequently observed adverse reactions to metronidazole include nausea, vomiting, cramps, diarrhea, and a metallic taste.The urine is often dark or redbrown. Less frequently, unsteadiness, vertigo, ataxia, paresthesias, peripheral neuropathy, encephalopathy, and neutropenia have been reported. Since metronidazole is a weak inhibitor of alcohol dehydrogenase, alcohol ingestion should be avoided during treatment. A psychotic reaction also may be produced. Metronidazole interferes with the metabolism of warfarin and may potentiate its anticoagulant activity. Phenobarbital and corticosteroids lower metronidazole plasma levels by increasing its metabolism, whereas cimetidine raises levels by impairing metronidazole metabolism.The drug is not recommended for use during pregnancy.
Safety Profile
Confirmed carcinogen with experimental carcinogenic, neoplastigenic, tumorigenic, and teratogenic data. Moderately toxic by ingestion, intraperitoneal, and subcutaneous routes. Human systemic effects by ingestion: paresthesia, nerve or sheath structural changes, eye changes, tremors, fever, jaundice and other liver changes, hearingacuity changes, somnolence, and ataxia. Experimental reproductive effects. Human mutation data reported. When heated to decomposition it emits toxic fumes of NOx.
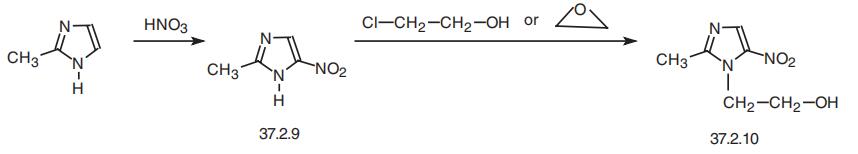
Synthesis
Metronidazole, 2-methyl-5-nitroimidazol-1-ethanol (37.2.10), is made by nitrating 2-methylimidazole to make 2-methyl-5-nitroimidazole (37.2.9), which is then reacted with 2-chloroethanol or ethylenoxide, which is easily transformed to the desired metronidazole.
Potential Exposure
Metronidazole is an orally administered drug for the treatment of infections due to entamoeba histolytica; trichomonas vaginalis; giardia lamblia, and has also been used for treating Vincent’s infection. It can be used as a trichomonacide in veterinary medicine. One firm has petitioned EPA to use metronidazole as a disinfectant for cooling tower water.
Veterinary Drugs and Treatments
Although there are no veterinary-approved metronidazole products,
the drug has been used extensively in the treatment of Giardia in
both dogs and cats. It is also used clinically in small animals for the
treatment of other parasites (Trichomonas and Balantidium coli) as
well as treating
both enteric and systemic anaerobic infections.
In horses, metronidazole has been used clinically for the treatment
of anaerobic infections.
Drug interactions
Potentially hazardous interactions with other drugs
Alcohol: disulfiram-like reaction.
Anticoagulants: effects of coumarins enhanced.
Antiepileptics: metabolism of phenytoin inhibited;
concentration reduced by phenobarbital.
Busulfan: concentration of busulfan increased - risk
of toxicity.
Ciclosporin: raised blood level of ciclosporin.
Cytotoxics: busulfan concentration increased;
metabolism of fluorouracil inhibited.
First aid
Skin Contacrt521: Flood all areas of body thathave contacted the substance with water. Do not wait toremove contaminated clothing; do it under the water stream.Use soap to help assure removal.I Isolate contaminatedclothing when removed to prevent contact by others. EyeContact: Remove any contact lenses at once. Flush eyeswell with copious quantities of water or normal saline for atleast 20- 30 min. Seek medical attention. Inhalation: Leavearea immediately; breathe fresh air. Proper respiratory pro-tection must be supplied to any rescuers. If coughing, diffi-cult breathing, or any other symptoms develop, seekmedical attention at once, even if symptoms develop manyhours after exposure. Ingestion: If convulsions are not pres-ent, give a glass or two of water or milk to dilute the sub-stance. Assure that the person's airway is unobstructed andcontact a hospital or poison center immediately for adviceon whether or not to induce vomiting.
Carcinogenicity
Metronidazole is reasonably anticipated to be a human carcinogenbased on sufficient evidence of carcinogenicity from studies in experimental animals.
Environmental Fate
Due to metronidazole’s use as a pesticide, it may have been directly released into the environment. It lacks an adequate chromophore for absorbing light and undergoing photolytic degradation. In addition, in vitro assays demonstrated the compound’s robust stability in the atmosphere or aqueous environments. Metronidazole exhibited a soil half-life between 10 and 27 days.
Metabolism
Metronidazole undergoes hepatic metabolism via hydroxylation, oxidation, and glucuronidation. The metabolism of metronidazole yields 5 metabolites. The hydroxy metabolite, 1-(2-hydroxy-ethyl)-2-hydroxy methyl-5-nitroimidazole, is considered the major active metabolite. Unchanged metronidazole is found in the plasma along with small amounts of its 2- hydroxymethyl metabolite. Several metabolites of metronidazole are found in the urine. They are primarily a product of side-chain oxidation in addition to glucuronide conjugation. Only 20% of the dose found in the urine is accounted for by unchanged metronidazole. The two main oxidative metabolites of metronidazole are hydroxy and acetic acid metabolites.
Metabolism
Metronidazole is available in a variety of dosage forms, including IV, oral, rectal, and vaginal
suppositories. The bioavailability of metronidazole is nearly 100% when administered orally but is
significantly less when administered via the rectal route (67–82%) or the vaginal route (19–56%).
The drug is not bound to plasma protein. Distribution of the drug is fairly uniform through out the
body, including mother's milk.
Liver metabolism of metronidazole leads to two major metabolites: hydroxylation of the 2-methyl
group to 2-hydroxymethylmetronidazole (HM), and oxidation to metronidazole acetic acid. Both
compounds possess biological activity. Additionally, HM is found in the urine as glucuronide and
sulfate conjugates. In addition, a small amount of metronidazole is oxidized to acetamide, a known
carcinogen in rats but not in humans.
Storage
Color Code—Blue: Health Hazard/Poison: Storein a secure poison location. Prior to working with thischemical you should be trained on its proper handling andstorage. Store in a refrigerator. A regulated, marked areashould be established where this chemical is handled, used,or stored in compliance with OSHA Standard 1910.1045.
Shipping
UN3249 Medicine, solid, toxic, n.o.s., Hazard Class: 6.1; Labels: 6.1-Poisonous materials.
Toxicity evaluation
Metronidazole is a prodrug that requires reductive activation of the nitro group by susceptible organisms. The reduction causes nitro radical formation and destruction of the organism’s DNA. The mechanism of neurotoxicity is thought to be due to axonal degeneration. Metronidazole has been shown to bind neuronal RNA in rodent models, thus inhibiting protein synthesis and causing degeneration. Metronidazole is also capable of producing a disulfiram-type reaction with ethanol ingestion. This reaction is hypothesized to occur due to metronidazole inhibition of aldehyde dehydrogenase.
Incompatibilities
Incompatible with oxidizers (chlorates, nitrates, peroxides, permanganates, perchlorates, chlorine, bromine, fluorine, etc.); contact may cause fires or explosions. Keep away from alkaline materials, strong bases, strong acids, oxoacids, epoxides.
Waste Disposal
Dispose of contents and container to an approved waste disposal plant. All federal, state, and local environmental regulations must be observed. It is inappropriate and possibly dangerous to the environment to dispose of expired or waste drugs and pharmaceuticals by flushing them down the toilet or discarding them to the trash. Household quantities of expired or waste pharmaceuticals may be mixed with wet cat litter or coffee grounds, doublebagged in plastic, discard in trash. Larger quantities shall carefully take into consideration applicable DEA, EPA, and FDA regulations. If possible return the pharmaceutical to the manufacturer for proper disposal being careful to properly label and securely package the material. Alternatively, the waste pharmaceutical shall be labeled, securely packaged, and transported by a state licensed medical waste contractor to dispose by burial in a licensed hazardous or toxic waste landfill or incinerator.
Properties of Metronidazole
| Melting point: | 159-161 °C (lit.) |
| Boiling point: | 301.12°C (rough estimate) |
| Density | 1.3994 (rough estimate) |
| refractive index | 1.5800 (estimate) |
| Flash point: | 9℃ |
| storage temp. | 2-8°C |
| solubility | acetic acid: 0.1 M, clear, faintly yellow |
| form | crystalline |
| pka | pKa 2.62(H2O,t =25±0.2,Iundefined) (Uncertain) |
| color | white to light yellow |
| Water Solubility | <0.1 g/100 mL at 20 ºC |
| Merck | 14,6157 |
| BRN | 611683 |
| Stability: | Stable. Incompatible with strong oxidizing agents. |
| NIST Chemistry Reference | Metronidazole(443-48-1) |
| IARC | 2B (Vol. 13, Sup 7) 1987 |
| EPA Substance Registry System | Metronidazole (443-48-1) |
Safety information for Metronidazole
| Signal word | Danger |
| Pictogram(s) |
 Health Hazard GHS08 |
| GHS Hazard Statements |
H340:Germ cell mutagenicity H350:Carcinogenicity H373:Specific target organ toxicity, repeated exposure |
| Precautionary Statement Codes |
P202:Do not handle until all safety precautions have been read and understood. P260:Do not breathe dust/fume/gas/mist/vapours/spray. P280:Wear protective gloves/protective clothing/eye protection/face protection. P308+P313:IF exposed or concerned: Get medical advice/attention. P405:Store locked up. P501:Dispose of contents/container to..… |
Computed Descriptors for Metronidazole
| InChIKey | VAOCPAMSLUNLGC-UHFFFAOYSA-N |
Metronidazole manufacturer
New Products
4,4-Difluoropiperidine hydrochloride tert-butyl 9-methoxy-3-azaspiro[5.5]undecane-3-carboxylate Indole Methyl Resin N-Isopropylurea N,N-Dicyclohexylcarbodiimide(DCC) MELDRUMS ACID 5-METHYLISOXAZOLE-4-CARBOXYLIC ACID Magnessium Bis glycinate Zinc ascorbate 1-bromo-2-butyne 2-acetamidophenol 9(10H)-anthracenone Erythrosin B, 4-Piperidinopiperidine 2-((4-morpholinophenylamino) (methylthio) methylene) malononitrile 2,4-dihydroxybenzaldehyde 3-(4-morpholinophenylamino)-5-amino-1H-pyrazole-4-carbonitrile Methyl 2-methylquinoline-6-carboxylate 2,6-dichloro-4-nitropyridine 4-Bromo-2-chlorobenzonitrile 2-(benzylamino)acetic acid hydrochloride 4-(tert-Butoxycarbonylamino)but- 2-ynoic acid 3,4-dihydro-2H-benzo[b][1,4]dioxepine 1-Phenyl-1-cycloprppanecarboxylicacidRelated products of tetrahydrofuran

You may like
-
 Metronidazole 99%View Details
Metronidazole 99%View Details -
 METRONIDAZOLE 95-99%View Details
METRONIDAZOLE 95-99%View Details
443-48-1 -
 Metronidazole 98% CAS 443-48-1View Details
Metronidazole 98% CAS 443-48-1View Details
443-48-1 -
 2-Methyl-5-nitroimidazole-1-ethanol CAS 443-48-1View Details
2-Methyl-5-nitroimidazole-1-ethanol CAS 443-48-1View Details
443-48-1 -
 Metronidazole CAS 443-48-1View Details
Metronidazole CAS 443-48-1View Details
443-48-1 -
 Metronidazole CAS 443-48-1View Details
Metronidazole CAS 443-48-1View Details
443-48-1 -
 Metronidazole CAS 443-48-1View Details
Metronidazole CAS 443-48-1View Details
443-48-1 -
 Metronidazole CAS 443-48-1View Details
Metronidazole CAS 443-48-1View Details
443-48-1
